Brain Tumour Group,Genito-Urinary Cancers Group,Head and Neck Cancer Group,News,Press release,Quality of Life Group,Soft Tissue and Bone Sarcoma Group
New results and forthcoming trials presented at ESMO 2025 underline EORTC’s commitment to patient-centred research
21 Oct 2025
Important new results and future trials were reported at the 2025 ESMO Congress held in Berlin from 17-21 October, further underlining the extent of EORTC’s commitment to innovative, independent cancer research.
- What happens when patients stop treatment during trials?
- Better ways of involving patients in research
- Understanding long-term survival in glioblastoma
- Two new trials will study individualised treatments in genitourinary cancers
- Searching for new treatments for adult fibrosarcoma patients
- Better ways of measuring quality of life
- New trials in head and neck and renal cancers
- Finally…
What happens when patients stop treatment during trials?
Many cancer clinical trial do not clearly report what happens to patients who stop their assigned treatment, and this raises concerns about the efficacy of experimental agents on long-term outcomes, according to results from a study presented by Dr Eva Blondeaux1. The researchers looked at 533 Phase II and III trials published between 2015 and 2024 that tested first-line treatments for solid tumours, and focused on two key measures: treatment discontinuation, when patients stop taking the drug, and attrition, when they receive no further treatment after so doing. Most of the trials included were industry-funded (54%) and Phase III (56%), and mainly involved patients with non-small cell lung cancer, breast cancer, and colorectal cancer.
More than three-quarters (78%) of the trials reported discontinuation rates, though only about half reported what treatments, if any, patients subsequently received. The median attrition rate was 38%, meaning that more than one in three patients stopped treatment without receiving any further therapy. Attrition rates varied by cancer type, with trials enrolling patients with urothelial cancer – where a tumour develops in the cells lining the urinary tract – showing the highest rate at 53%, while trials enrolling patients with breast cancer had the lowest (22%). The researchers found that attrition rates in industry-sponsored trials were higher, at 39%, than in academic trials (31%).
The findings show that while most cancer trials show how many patients stop treatment, they often do not provide enough information about what happens to those patients afterward,” says Dr Blondeaux. “Without these data, it is difficult to deeply understand the long-term impact of new cancer therapies.”
Simulations of different attrition rates indicated that if an imbalance between treatment arms in the percentage of patients receiving a subsequent treatment occurs, statistically significant results in overall survival are more likely to be observed, leading to an overestimate of treatment effect. This is particularly noticeable when more patients in the experimental arm receive a subsequent treatment compared with patients receiving the standard treatment.
Better ways of involving patients in research
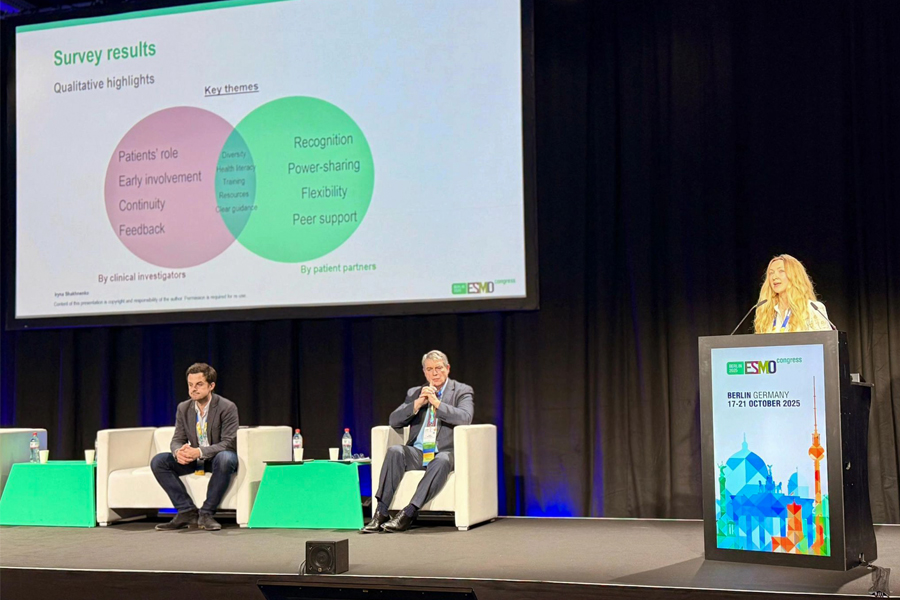

Involvement of patients and caregivers in oncology research is essential, both for the conduct of the research and for obtaining robust results. However, its success depends on the commitment and structured approach of research organisations. Iryna Shakhnenko2 presented the results of an EORTC survey that aimed to identify the challenges involved and to address key elements for the future patient involvement framework. A literature review revealed many frameworks for patient involvement, but most were ungeneralisable.
“This highlighted the need for a flexible framework that would be more suitable for EORTC’s research environment,” she said.
Patients, caregivers, researchers, and clinical investigators were asked for their views on elements including engagement principles, training needs, patients partner’s roles and workload, a patient advisory board, and strategies for monitoring and assessing impact. Nearly 66% of clinical investigators and 62% of patient partners responded that they lacked guidance on patient involvement. While 80% of researchers sought documented patient involvement plans, 79% of patient partners stressed the need for clear methods of evaluating impact.
These insights have the potential to offer practical solutions for patient and caregiver involvement across EORTC and other cancer research organisations, the researchers say.
Understanding long-term survival in glioblastoma
The ETERNITY (EORTC 1419)3 study is the largest registry of long-term glioblastoma survivors worldwide. Glioblastoma is the most aggressive type of brain tumour, and life expectancy after diagnosis is usually short, with a median survival time of 12 months. In a new analysis presented at the conference by Professor Michael Weller, researchers described the findings of their study of tumour samples from 130 patients who lived at least five years after diagnosis, comparing them to data from other glioblastoma cohorts in an attempt to understand the reasons why they survived for so much longer than the average.
They found that the long-term survivors had tumours that fell into recognised molecular subtypes, with an enrichment in a subtype that is highly aggressive, spreads easily, and involves inflammation. and fewer tumours in a subclass that grows rapidly due uncontrolled cell division. They also found a high frequency of a tumour marker (MGMT promoter methylation) that makes cancer cells more sensitive to chemotherapy and therefore improves response to treatment. While alterations in the structure or number of chromosomes in the long-term survivors were similar to those found in the tumours of other patients, they were more likely to have specific genetic deletions from the long arm of chromosome 10 involving the MGMT gene. While there were other small differences in mutations between the two groups, the tumours of the long-term survivors showed no unique molecular signatures. This suggests that survival may be influenced by many different factors, the researchers say.
“Glioblastoma is an extremely challenging disease, but understanding this particular subgroup of survivors can help us devise research and treatment strategies that may be applicable more widely, and extend survival for greater numbers of patients,” said Prof Weller.
Two new trials will study individualised treatments in genitourinary cancers
A new international study that will investigate whether men with metastatic hormone-naïve prostate cancer can safely interrupt treatment with androgen deprivation therapy (ADT) and androgen receptor pathway inhibitors (ARPI) once they respond well, rather than continuing therapy indefinitely, was presented by Dr Guillaume Grisay. The DE-ESCALATE trial4 will validate the benefits of giving intermittent androgen deprivation treatment in metastatic hormone-naïve prostate cancer, attempting to improve patients’ quality of life while preserving survival. The investigators believe that this Europe-wide pragmatic clinical trial, involving a diversity of patients in a real-world setting, will show that a significant volume of drugs could be spared, thus providing benefits to both patients’ quality of life and healthcare systems.
Despite intensive screening for prostate cancer, some patients do not present until they are at the metastatic stage and the usual treatment, while increasing overall survival, does not come without toxicity. This means that the patient pays a very high price, with chronic and sometimes serious side effects. Optimisation trials over the past 20 years have shown that patients treated with androgen deprivation (ADT) could only be offered intermittent therapy, the pausing of the ADT, once their PSA reaches a sufficiently low level. This treatment interruption significantly increases quality of life, and is called intermittent androgen deprivation (IAD) therapy.
This was a standard of care until the advent of ARPI, since when treatment has been administered continuously. As ADT + ARPI significantly increase the percentage of patients with a profound response, there is an even higher proportion of patients who would be candidates for the intermittent approach. If intermittent treatment proves to be as safe and effective as continuous therapy, it could reduce long-term side effects, improve quality of life, and ease treatment costs for patients and healthcare systems alike. The trial thus represents an important step toward more personalised care in prostate cancer.
The study opened in Croatia, Denmark, Ireland, France, and Spain in June 2025, with additional countries—including Belgium, Portugal, Italy, Romania, Slovenia, Switzerland, and the Czech Republic—expected to join in 2026.
A second new, international trial that will investigate an innovative approach to tackling muscle-invasive bladder cancer (MIBC), a serious form of cancer that often requires major surgery, was presented by Dr Julien Van Damme. The STARBURST-1 trial5 will focus on the development of a reliable molecular signature that can predict whether or not a patient will have a complete response to treatment. Currently, standard treatment for MIBC consists of pre-operative (“neoadjuvant”) systemic therapy (NAT) followed by either radical cystectomy (RC), the complete removal of the bladder, or a combination of therapies that allows the bladder to be spared (trimodal therapy or TMT). However, patients are not routinely assessed after NAT, and this means that those who have had a good response to the therapy may receive unnecessary treatment with a subsequent impact on their quality of life.
STARBURST-1 will enrol patients with newly-diagnosed MIBC, all of whom will receive NAT followed by an RC. Before starting treatment, patients will be evaluated via blood and urine biomarkers and imaging. After treatment, patients will undergo similar tests, including MRI, to see how they responded to the treatment. The results will be assessed with NacVI-RADS, an MRI scoring system to describe cancer response to treatment, and analyses will reflect whether this score had predicted the outcome correctly when comparing pre and post treatment MRI scans. Should this be the case, a second phase of the trial, STARBURST-2, will then test strategies adapted to the individual patient’s response to NAT, with the aim of ascertaining who still needs major surgery and who can safely avoid it. In addition, being able to identify patients who have not responded at an earlier stage will mean that they can be offered immediate treatment adapted to their individual circumstances.
Searching for new treatments for adult fibrosarcoma patients
Adult fibrosarcoma (AF)is a very rare, aggressive form of soft tissue sarcoma and little is known about how effective current treatments are for patients. Dr Fernando Campos6, from the EORTC Soft Tissue and Bone Sarcoma Group presented the largest analysis to date of how patients with adult fibrosarcoma (AF) respond to first-line chemotherapy.
The study looked at 51 people with inoperable, metastatic AF who had taken part in seven clinical trials since 1990. Chemotherapy, usually with anthracycline-based drugs, is often the standard first treatment for soft tissue sarcomas. However, these new results showed that in AF its benefits are limited. Only a small number of patients (about 8%) saw their tumours shrink. Just over half (57%) had their disease remain stable for a time, while nearly a third (31%) experienced further progression despite treatment. On average, patients lived for about 12 months after starting chemotherapy, with disease control lasting a median time of only three months.
“These results highlight how challenging adult fibrosarcoma is to treat with existing chemotherapy options,” said Dr Campos. “Because this cancer is so rare, progress can only come from international collaboration and pooling data across studies. We hope that our findings will encourage further collaborative research in this neglected area.”
Better ways of measuring quality of life
Veronika Engele, MSc, presented a new questionnaire designed to measure the quality of life (QOL) in individuals with hereditary cancer risk, both with and without cancer. People who inherit gene variations known to increase the risk for cancer onset – so called hereditary cancer predisposition syndromes – often face emotional, social, and physical QOL impairments. Given the rapid advances in this field, researchers say that there is a clear need for a targeted patient-reported outcome questionnaire specifically designed to systematically assess QOL in this group.
An international group of researchers collaborated in the development process of EORTC hereditary cancer risk QOL questionnaire. After reviewing hundreds of scientific papers, both individuals with hereditary cancer risk and healthcare professionals were interviewed to identify the most relevant and important QOL issues. Early versions of the questionnaire were tested in multiple languages with participants from nine countries resulting in a final set of 30 questions forming the EORTC QLQ-HCR30 questionnaire.
The questionnaire captures key QOL issues relevant for individuals with hereditary cancer risk and is ready for the next step in the development process – evaluating its performance in larger studies.
Dr Louis Fox presented the results of an international research team’s review of over 170 studies and interviews with both patients and healthcare professionals to try to identify what really matters to people taking immune checkpoint inhibitorsa (ICIs). ICIs are revolutionising cancer treatment, helping many patients live longer. However, they can also cause unique and sometimes long-lasting side effects that affect daily life, mood, and relationships. Existing quality of life questionnaires may not fully capture these experiences.
They amassed 147 possible quality of life issues, refined them through interviews and surveys with more than 150 patients with various cancers, and narrowed the list to 42 key issues; many of which were not covered in existing questionnaires.
The researchers say that this new list will guide the creation of better tools to measure how immunotherapy affects patients’ lives—helping doctors, researchers, and policymakers improve care and make treatment decisions that reflect what patients value most.
a Drugs that prevent the immune system from switching off and help it to find and attack cancer cells
New trials in head and neck and renal cancers
Dr Irene Braña introduced the randomised Phase III EORTC 2014-HNCG PROLoNg trial of Pembrolizumab and radiotherapy for oligometastaticb squamous cell carcinoma of the head and neck (cancer of the mouth, throat, or larynx). The trial will be launched this year in Belgium, Italy, Spain, and Switzerland, and will be the first multicentric, international effort aiming to provide high level evidence for the combined approach of stereotactic ablative radiotherapy (SABR – a highly directed form of radiotherapy that delivers a high dose to the tumour while sparing surrounding healthy tissues) and immune checkpoint inhibitors for oligometastatic squamous cell carcinomas of the head and neck.
The RENALUT trial was presented by Dr Emmanuel Seront. Standard treatments often stop working after a while in people with advanced clear cell renal cell carcinoma, a type of kidney cancer. The trial is exploring a new treatment – radioligand therapy – that delivers radiation directly to cancer cells.
The trial is testing a radioligand drug, Lu-PSMA-617, that targets the PSMA protein, which is found in high amounts in kidney cancer blood vessels. This same drug has shown promising results and good safety in men with advanced prostate cancer. The study will include people whose cancer has worsened despite previous treatments, and whose scans show PSMA-positive tumours.
This Phase 2 study will measure how effective and safe the treatment is. Researchers hope it will provide a new treatment option for patients who currently have few remaining choices, and help to extend their survival.
b A type of metastasis in which cancer cells from the primary tumour travel through the body and form a small number of new tumours in one or two other parts of the body. This limited spread means that there is still a potential for cure, whereas this is seldom the case in tumours that have metastasised more widely.
Finally…
EORTC staff spoke at three special sessions. Dr Madeline Pe, Head of the Quality of Life Department, presented highlights from the final recommendations from the SISAQOL-IMI7 consortium during the ESMO-MCBS session ‘From Evidence to Reimbursement’. SISAQOL stands for Setting International Standards in analysing patient-reported outcomes and Quality Of Life endpoints. It is a global, multi-stakeholder, and multidisciplinary consortium that brings together representatives from regulatory and health technology assessment bodies, industry, academia and patients , with a shared interest of improving standards on the design, analysis, presentation and interpretation of health-related quality of life and PRO data in cancer clinical trials. The consensus recommendations are practice-changing and will help elevate PRO endpoints to the same level as other clinical endpoints, she says.
Dr Denis Lacombe8, CEO, spoke about treatment optimisation from the perspective of a healthcare provider and trialist, exploring the value of clinical trials that further document the optimal use of therapeutic interventions. Treatment optimisation can lead to the strategic revisiting of the continuum of the development of new technologies, he said. He discussed policy actions that could lead to treatment optimisation becoming integral to the pathway between research and clinical application.
Dr Lacombe also spoke on diversity, equity, and inclusion in clinical trials. Delivering clinical trials where the results can be safely applied to the majority of patients is a high societal priority. But conducting such trials addressing patient management and the utilisation of therapeutic interventions does not come without challenges, he said, calling for new approaches and partnerships to become part of the search for the provision of therapeutic progress for all.
Related News
EORTC Quality of Life Group participating at the ISOQOL 2025 Conference
22 Oct 2025
EORTC celebrates the 100th anniversary of p-value on World Statistics Day
20 Oct 2025
EORTC Announces Final Overall Survival Results from the PEACE-3 Trial
19 Oct 2025
Results from EORTC trial define new standard of care for aggressive brain tumours
18 Oct 2025
EORTC’s presence at ESMO 2025
17 Oct 2025
EORTC’s presence at EANO 2025
16 Oct 2025
EORTC celebrates Pink October: shaping the future of breast cancer care
15 Oct 2025
EORTC shines a light on advancements in radioligand therapy
8 Oct 2025
Treatment optimisation: making cancer treatment accessible and sustainable in Europe
24 Sep 2025
EORTC celebrates World Radiotherapy Awareness Day (WRAD) through innovation and collaboration in clinical cancer trials
3 Sep 2025


