Since 1962, EORTC has enrolled more than 205,000 patients in practice-changing trials across tumour types. Many of these trials have changed best practice for treating patients, with truly life-changing & life-saving results. EORTC’s trial protocols have been adopted as best practice in many countries, and are used in the US, Canada, Australia & elsewhere.
EORTC clinical trials transform the lives of patients & their families and save healthcare systems millions – without any commercial interest at stake.
Brain Tumours
 Brain cancer: a rare and deadly type of cancer
Brain cancer: a rare and deadly type of cancer
Brain cancer accounts for approximately 3% of all cancer cases worldwide1. Generally, around 17 out of every 100 people with a cancerous brain tumour will survive for 5 years or more after being diagnosed2.
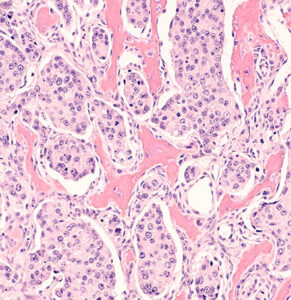
Brain tumours encompass many different cancer types. Primary brain tumours originate from the brain tissue itself, while secondary brain tumours are metastases spreading to the brain from cancers of other organs (e.g. lung cancer, breast cancer, melanoma).
Despite decades of research, brain tumours remain among the deadliest of all forms of cancer. The ability of these tumours to resist almost all conventional and novel treatments relates, in part, to the unique cell-intrinsic and microenvironmental properties of neural tissues3.
EORTC Brain Tumour Group: setting the standards of treatment
The EORTC Brain Tumour Group conducts research on several types of brain tumours of adults with the goal to improve treatments for and outcomes of glioblastoma patients. The current standard of care therapy for several glioma types was defined by clinical trials led by the Group, and involves neurosurgery, radiotherapy and chemotherapy. Current trial activities aim to test novel treatment approaches such as investigational agents and combined treatment modalities.
1 2. Ferlay J, Seorjomataram I, Ervik M, et al. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11 [Internet]. Lyon, France: International Agency for Research on Cancer; 2013. Available from: http://globocan.iarc.fr. Accessed May 30, 2016. [Google Scholar] [Ref list]
2 3. Ohgaki H. Epidemiology of brain tumors. Methods Mol Biol Clifton NJ. 2009;472:323–342. doi:10.1007/978-1-60327-492-0_14. [PubMed] [Google Scholar] [Ref list]
3 Aldape K, Brindle KM, Chesler L, Chopra R, Gajjar A, Gilbert MR, Gottardo N, Gutmann DH, Hargrave D, Holland EC, Jones DTW, Joyce JA, Kearns P, Kieran MW, Mellinghoff IK, Merchant M, Pfister SM, Pollard SM, Ramaswamy V, Rich JN, Robinson GW, Rowitch DH, Sampson JH, Taylor MD, Workman P, Gilbertson RJ. Challenges to curing primary brain tumours. Nat Rev Clin Oncol. 2019 Aug;16(8):509-520. doi: 10.1038/s41571-019-0177-5. PMID: 30733593; PMCID: PMC6650350.
 Introducing personalised treatment for brain cancer.
Introducing personalised treatment for brain cancer.
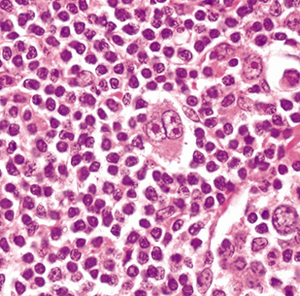
Glioblastoma is an aggressive and lethal type of brain cancer that appears in people of all ages. According to the World Health Organisation, glioblastomas are classified as Grade IV and represent (along with grade III gliomas) the majority of brain tumours [1]. Overall, glioblastomas incidence is 1 per 10 000 cases among all cancer types. However, they represent 16% of all primary brain tumours, making them the most common brain cancer and almost always the most lethal [2, 3, 4]. Today, long-term glioblastoma survivors are defined as patients who live longer than 2 years following their diagnosis whereas extreme survivors, living 10 years or more, account for 1% of all patients [5]. This EORTC trial was instrumental to the prolonged survival of glioblastoma patients and remains the standard of care to this date.
Prior to this EORTC trial, the only available treatment involved surgery to remove the tumour followed by radiotherapy of the brain. This treatment however had very little impact on patients’ survival.
The EORTC trial successfully showed that a drug called temozolomide, when taken as a pill after surgery and in addition to radiotherapy, allowed many patients to live longer. In addition, taking this pill did not cause too many adverse effects to patients, who reported on average that their quality of life was not worse than that reported by the patients not taking the drug. Since a large number of patients saw an improvement by taking this drug, researchers tried to identify ways they could predict which patients would benefit (i.e., live longer) from this treatment and which have less chance of doing so. They succeeded in identifying a gene as the first predictive marker in brain tumours (called MGMT promoter methylation) associated with a better response to the treatment. To date, this molecular test is used in all patients with glioblastoma and was the one that introduced the concept of personalised treatment in neuro-oncology. This personalised combination treatment became the standard of care for newly diagnosed glioblastoma patients worldwide.
Nomograms for predicting survival of patients with newly diagnosed glioblastoma: prognostic factor analysis of EORTC and NCIC trial 26981-22981/CE.3 Gorlia T, van den Bent MJ, Hegi ME, et al.
Lancet Oncol 2008 Jan;9(1):29-38.
 Improving survival of brain tumour patients by effectively combining radiotherapy & chemotherapy.
Improving survival of brain tumour patients by effectively combining radiotherapy & chemotherapy.
Anaplastic gliomas are a rare type of brain tumours. Every year, just 1 in 100,000 people is diagnosed with this cancer [1]. In the majority of these cases, between 70% to 80%, the patients have a specific gene change (called the IDH gene). When the trial was designed, it was clear that the chemotherapy drug temozolomide (TMZ for short) increased survival in patients with grade 4 brain tumours (gliomas).
However, for patients with grade 3 brain tumours (gliomas) that had this mutation of the IDH gene, this chemotherapy did not yield the same positive results.
The trial successfully showed that when grade 3 patients are given a combination treatment in a specific order – with radiotherapy first, followed by administering the drug temozolomide – their survival rate doubles.
This has been an important study in the field of brain tumours providing a significant increase in the survival of patients with anaplastic gliomas to date.
Adjuvant and concurrent temozolomide for 1p/19q non-co-deleted anaplastic glioma (CATNON; EORTC study 26053-22054): second interim analysis of a randomised, open-label, phase 3 study.
van den Bent MJ, Tesileanu CMS, Wick W, et al.
Lancet Oncol 2021 Jun;22(6):813-23.
Breast Cancer
 Breast Cancer
Breast Cancer
Breast cancer is the most commonly diagnosed cancer in women and the most common cause of cancer death in women worldwide (1 in 6 cancer deaths) [1]. According to WHO, in 2020, there were 2.3 million women diagnosed with breast cancer [2]. Incidence rates vary across countries. In a developed country setting, about 1 in 8 women will be diagnosed with breast cancer in their lifetime [1].
Early-stage breast cancer is defined as disease confined in the breast (lump of size up to 5cm) and / or regional lymph nodes, without distant metastases (spread of cancer to other organs). With treatment, women with early breast cancer have a very good prognosis (chance of survival). The primary treatment (core treatment) for early breast cancer is surgery. Reducing the chances of recurrence and therefore increasing the survival rate of these patients, means additional treatment (chemotherapy and /or radiotherapy) after surgery. These additional treatments bear toxicities for the human body and researchers aim to find ways of reducing/limiting these adverse effects and thus increasing their quality of life, without affecting their chances of survival.
The following three EORTC Breast Cancer Group clinical trials are examples of reducing treatment without compromising patients’ survival rates (very good prognosis) but having a significant increase in their quality of life.
 Using gene signatures to determine optimal treatment in early breast cancer.
Using gene signatures to determine optimal treatment in early breast cancer.
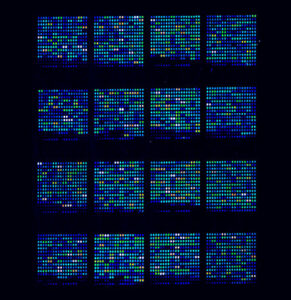
Studies over the years have shown that treating women diagnosed with early breast cancer with chemotherapy after surgery, has significant results in their overall survival. Chemotherapy however can negatively affect patients’ overall health and quality of life in the long term. The EORTC MINDACT study sought to investigate whether women diagnosed with early breast cancer that hasn’t spread beyond the breast and/or the nearby lymph nodes (masses of tissue that help the body to fight disease), could be spared chemotherapy treatment after surgery, without affecting their overall survival rate.
This led to the development of a test, called MammaPrint® which examines the profile of 70 different genes and determines which patients bear genomic low risk and can therefore avoid chemotherapy. This was the first effective tool of its kind in assessing the prognosis of these patients.
The study found that 94.7% of women who were identified as genomic low risk using the 70 gene signature test, and therefore did not receive chemotherapy, were free of disease 5 years later.
Long-term monitoring of these patients at 8.7 years confirmed the initial trial results and found that 95.1% were free of disease and free of metastasis (disease spread) after 5 years. The EORTC MINDACT trial has proven instrumental in reducing treatment where possible and paving the way towards optimised care and quality of life for patients.
70-gene signature as an aid for treatment decisions in early breast cancer: updated results of the phase 3 randomised MINDACT trial with an exploratory analysis by age.
Piccart M, van ‘t Veer LJ, Poncet C, et al.
Lancet Oncol 2021 Apr;22(4):476-88.
 Sparing women with early breast cancer from mastectomy.
Sparing women with early breast cancer from mastectomy.
This EORTC clinical trial was part of a series of trials that proved that breast conserving treatment can be used in certain women diagnosed with early breast cancer instead of mastectomy (removal of the breast).
It proved that patient survival was identical between the two treatment options. This is an important EORTC study, as it enabled to change the standard of practice by improving the patients’ quality of life while equally helping doctors to better inform their patients of their options.
To date, for most women diagnosed with early breast cancer, breast conservation treatment remains an option sparing them from medically unnecessary more extensive surgery (removal of the breast).
Breast conserving therapy versus mastectomy for stage I–II breast cancer: 20 year follow-up of the EORTC 10801 phase 3 randomised trial.
Litière S, Werutsky G, Fentiman IS, et al.
Lancet Oncol 2012 Apr;13(4):412-19.
 Confirming radiation as an effective treatment alternative to surgery, for women with early breast cancer.
Confirming radiation as an effective treatment alternative to surgery, for women with early breast cancer.
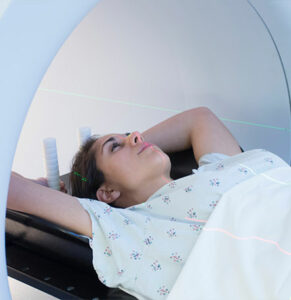
In women diagnosed with early breast cancer, the first step before deciding on a treatment is for doctors to assess whether the tumour has affected the lymph nodes (masses of tissue, part of the body’s immune system, that help the body to fight disease). This procedure is called sentinel node biopsy.
Most cases are negative, however, in the case of a positive biopsy, the lymph nodes are removed (called axillary dissection).
This nonetheless negatively impacts the quality of life of patients as removal of the lymph nodes close to the breast is associated with lifetime health complications (swelling of arm, pain etc) in the majority of cases.
The AMAROS study, sought to investigate whether in cases of a positive sentinel biopsy, radiation of the affected area could be an alternative to surgical removal and thus sparing women from permanent health complications following the surgical removal of the lymph nodes. The study found radiation to be an effective alternative to surgical removal in regional control of the tumour.
Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer (EORTC 10981-22023 AMAROS): a randomised, multicentre, open-label, phase 3 non-inferiority trial.
Donker M, van Tienhoven G, Straver ME, et al.
Lancet Oncol 2014 Nov;15(12):1303-10.
Genito-Urinary Cancers
 Prostate Cancer
Prostate Cancer
The prostate gland, found only in men, is situated between the bladder and the rectum.
Prostate cancer is the second most frequently occurring cancer in men, after lung cancer, and accounting for almost 1.4 million new cases and 375,000 deaths worldwide in 2020 [1]. It is the most frequently diagnosed male cancer in over half of the countries across the world.
Although the highest number of diagnoses are found in higher-income countries, deaths do not follow this pattern, with the highest number being found in the Caribbean, sub-Saharan Africa, and Micronesia/Polynesia. These differences are most likely due to the widespread introduction of screening in higher-income countries, which has allowed early detection.
Patients with prostate cancer that cannot be halted by lowering testosterone levels (castration-resistant cancer), and where the cancer has spread (metastasised) to their bones, are usually treated with the chemotherapy drugs Ra-223, enzalutamide, and abiraterone.
 Investigating the effect of adding bone-protection to chemotherapy for prostate cancer.
Investigating the effect of adding bone-protection to chemotherapy for prostate cancer.
Patients with prostate cancer that cannot be halted by lowering testosterone levels (castration-resistant cancer), and where the cancer has spread (metastasised) to their bones, are usually treated with the chemotherapy drugs Ra-223, enzalutamide, and abiraterone. Evidence indicated that giving Ra-223 together with one of the other two drugs as soon as bone metastases appeared might be beneficial. But an EORTC trial was halted when it became clear that giving Ra-223 with abiraterone significantly increased the risk of patients suffering bone fractures. Following this finding, new guidelines were issued stating that medication to protect the bones should be added whenever Ra-223 is given.
As a result, the PEACE III trial, which was comparing the outcomes of the use of Ra-223 plus enzalutamide with enzalutamide alone in castration-resistant patients with bone metastases, started to give bone-protecting agents to both groups.
The researchers were able to study results from the patients who had started treatment earlier, before the introduction of bone protection, and found that one year after treatment the risk of fracture in the group who received the drug combination was considerably higher than in those who received enzalutamide alone. However, they were also able to see that with the later addition of bone-protecting treatment, this risk had almost disappeared, and thus confirm that bone protection gives patients a better quality of life.
The PEACE III trial is continuing, and full results from the comparison of the two treatments plus bone protection will be available after it closes.
Decreased fracture rate by mandating bone-protecting agents in the EORTC 1333/PEACE III trial comparing enzalutamide and Ra223 versus enzalutamide alone: An interim safety analysis.
Tombal BF, Loriot Y, Saad F, et al.
J Clin Oncol 2019 May;37(15)Suppl:5007.
Head & Neck Cancer
 SCC of the Head & Neck
SCC of the Head & Neck
Squamous cell carcinoma (SCC) is the second most common skin cancer, the first being melanoma [1]. It begins in the squamous cells of the body. These thin, flat cells are found in the tissue that forms the epidermis, or outmost layer of the skin, as well as the lining of hollow organs and of the respiratory and digestive tracts. About 90% of head and neck cancers* are squamous cell carcinomas (SCCs).
SCC of the head and neck (HNSCC) is the sixth most common cancer worldwide, with 890,000 new cases and 450,000 deaths in 2018. The incidence of HNSCC continues to rise and is anticipated to increase by 30%, or 1.08 million new cases annually by 2030, according to Global Cancer Observatory (GLOBOCAN).
Currently only about half the patients with an HSNCC are still alive five years after their diagnosis. This is in part due to the fact that the majority of these patients consult at a late stage and already have cancer that has spread to their lymph nodes at the time they are diagnosed.
* Head & Neck cancer: Term used to describe a number of different cancers that develop in or around the throat, larynx, nose, sinuses, & mouth.
 Preserving natural speech in cancer of the head & neck with larynx-preserving radio-chemotherapy.
Preserving natural speech in cancer of the head & neck with larynx-preserving radio-chemotherapy.
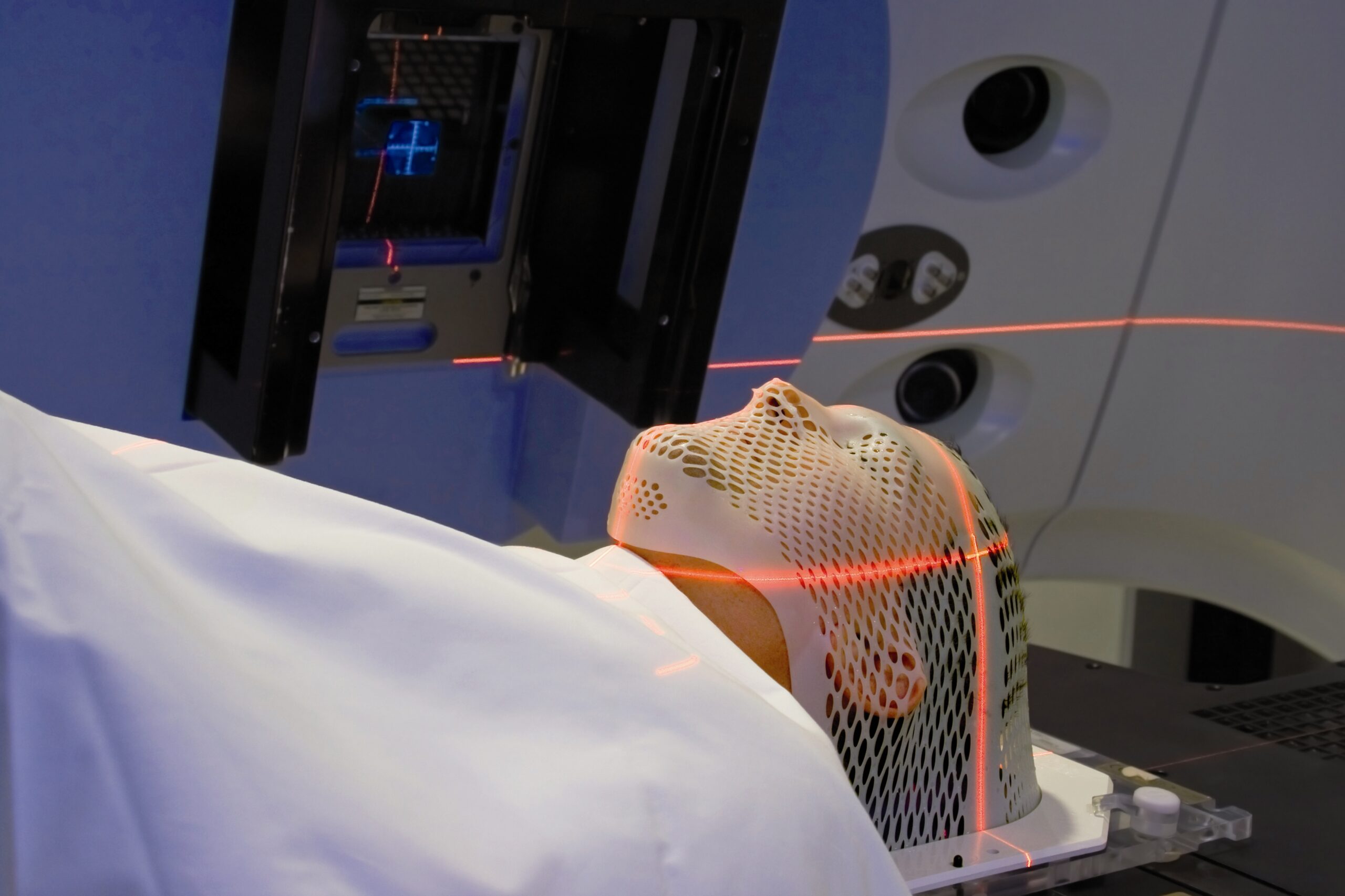
This trial was conducted in patients with laryngeal cancer – a form of SCC of the head and neck where tumour cells arise from the cells lining the inside of the larynx, which is the part of the throat that contains the vocal cords (the voice box). Previously, this type of cancer was treated either with surgery or radiotherapy*, both of which would frequently lead to patients losing their ability to speak, and thus have a significant impact on their quality of life. Later, chemotherapy** provided an alternative that could allow preservation of the larynx.
The trial compared these different approaches, and evaluated whether using chemotherapy combined with radiotherapy instead of surgery as initial treatments could be beneficial in a group of patients with hypopharyngeal SCC. The hypopharynx is situated at the bottom of the throat, just behind the larynx. It found that larynx-preserving treatment did not jeopardise overall survival in patients with SCC of the head and neck and allowed more than half of the survivors to retain their ability to speak. This, of course, made a huge difference to their daily lives. The results from this study changed the standard of care and practice for patients with early-stage hypopharyngeal SCC from larynx surgery to larynx-preserving radio-chemotherapy.
*Radiotherapy: Type of local cancer treatment that uses beams of intense energy to kill cancer cells. Radiotherapy damages cells by destroying the genetic material that controls how cells grow & divide. Normal cells such as those lining the inside of the mouth may also be affected by these treatments. This slows down the ability of oral tissue to repair itself and increases risk of side effects during treatment.
**Chemotherapy: Treatment that uses drugs to stop the growth of cancer cells that were not visible at time of surgery, by killing the cells or stopping them from dividing
Laryngeal preservation with induction chemotherapy for hypopharyngeal squamous cell carcinoma: 10-year results of EORTC trial 24891.
Lefebvre JL, Andry G, Chevalier D, et al. for the EORTC Head & Neck Cancer Group.
Annals Oncol 2012 Apr;23:2708-14.
 Improving survival in locally advanced head & neck cancer through combined radio-chemotherapy after surgery.
Improving survival in locally advanced head & neck cancer through combined radio-chemotherapy after surgery.
When HNSCC is at an advanced stage the cancer often comes back, either in the same place or close by, after surgery to remove the tumour. Cancer cells may also break away and form new tumours in other parts of the body (metastases). Additional treatment with radiotherapy* immediately after surgery may reduce or delay this to some extent.
Previous research had shown that combining post-operative radiotherapy with chemotherapy** might help stop the growth of the cancer at its original site (local control). This study looked at whether adding chemotherapy to radiotherapy after surgery when treating patients who were at high risk of their cancer returning could improve their survival.
It found that compared with radiotherapy alone, combined post-operative chemo-radiotherapy significantly increased the time patients spent without their disease getting worse (progression-free survival). After five years, this had increased by 11%, and the number of them still alive five years later (overall survival) was increased by 13%. This was an important improvement for these patients who were at high risk of a further deterioration in their cancer state, and today this combined approach is still the reference treatment for them.
*Radiotherapy: Type of local cancer treatment that uses beams of intense energy to kill cancer cells. Radiotherapy damages cells by destroying the genetic material that controls how cells grow & divide. Normal cells such as those lining the inside of the mouth may also be affected by these treatments. This slows down the ability of oral tissue to repair itself and increases risk of side effects during treatment.
**Chemotherapy: Treatment that uses drugs to stop the growth of cancer cells that were not visible at time of surgery, by killing the cells or stopping them from dividing.
Postoperative Irradiation with or without Concomitant Chemotherapy for Locally Advanced
Head and Neck Cancer.
Bernier J, Domenge C, Ozsahin M, Matuszewska K, et al. for the EORTC Trial 22931.
N Engl J Med 2004;350:1945-52.
Lung Cancer

Lung Cancer
Lung cancer is the leading cause of cancer deaths worldwide [1].
There are two main types of lung cancer: non-small cell lung cancer (85%) and small cell lung cancer (15%). Causes include passive and active smoking, exposure to certain toxins and family history. There are three subtypes of non-small cell lung cancer (NSCLC): adenocarcinoma, squamous cell carcinoma, and large cell carcinoma. Small cell lung cancer tends to grow and spread faster than NSCLC.
In past decades, there has been considerable progress in lung cancer care thanks to molecular profiling* making it possible to personalise treatment for each patient, to stimulate research, and to increase the portfolio of new treatment options.
Treatments may include surgery, chemotherapy, radiation therapy, targeted drug therapy and immunotherapy depending on the type of cancer, molecular profile and if disease spreads or not.
*Molecular testing use technologies to examine the patient’s DNA in order to identify changes that may cause cancer.
A randomised, phase 3 trial with anti-PD-1 monoclonal antibody pembrolizumab (MK-3475) versus placebo for patients with early stage NSCLC after resection and completion of standard adjuvant therapy (PEARLS) KEYNOTE-091.
This randomised, placebo-controlled, phase 3 trial recruited 1177 patients. Eligible patients were aged 18 years or older, with completely resected, pathologically confirmed stage IB (tumours of ≥4 cm in diameter), II, or IIIA NSCLC per the American Joint Committee on Cancer staging system (7th edition) of any histology or PD-L1 expression level, and an Eastern Cooperative Oncology Group performance status of 0 or 1; adjuvant chemotherapy was to be considered for stage IB disease and was strongly recommended for stage II and IIIA disease, according to national and local guidelines.
The statistical analysis showed that pembrolizumab improved significantly disease-free survival compared with placebo and was not associated with new safety signals in completely resected, PD-L1-unselected, stage IB–IIIA NSCLC.
Based on the above outcome:
1. In January 2023, the FDA approved pembrolizumab (Keytruda) for adjuvant treatment following resection and platinum-based chemotherapy for stage IB (T2a ≥4 cm), II, or IIIA non-small cell lung cancer (NSCLC).
2. In October 2023, the European Commission approved pembrolizumab (Keytruda) for the adjuvant treatment of adults with non-small cell lung carcinoma who are at high risk of recurrence following complete resection and platinum-based chemotherapy.
Lymphoma
 Lymphoma
Lymphoma
The EORTC Lymphoma group focuses on Hodgkin Lymphoma (HL), a rare cancer that accounts for 0.4% of all cancers and 0.2% of cancer deaths. HL originates from a specific type of white blood cell called lymphocytes. Treatment options for HL include chemotherapy, radiation therapy, and stem-cell transplantation, with the choice depending on the stage and characteristics of the cancer.
Despite being highly curable, with cure rates exceeding 80% using therapies combining chemotherapy and radiotherapy, long-term side effects and treatment-related toxicity pose challenges, increasing the risk of other cancers, heart disease, or lung disease. Patients with relapsed or refractory disease have unfavourable outcomes.
Recent advancements in treatment include the use of brentuximab vedotin for advanced disease and immune checkpoint inhibitors nivolumab and pembrolizumab for patients with relapsed/refractory disease.
The EORTC Lymphoma group is actively involved in various aspects of HL, including early and advanced stages, elderly population, and relapsed/refractory cases. They also conduct translational research and investigate the impact of the disease and treatment on long-term survivors in areas such as parenthood, education, work and insurance, and health and social situation.
 Treatment optimisation for Hodgkin Lymphoma: towards increasing efficacy or sparing toxicity, depending on each patient’s early response to treatment.
Treatment optimisation for Hodgkin Lymphoma: towards increasing efficacy or sparing toxicity, depending on each patient’s early response to treatment.
Treatment of early-stage Hodgkin lymphoma (HL), which consists of a combination of chemotherapy and radiotherapy (RT) [1,2] is extremely successful, with a cure rate of more than 90%. However, toxicities surfacing years following treatment are of major concern and mainly include second cancers [3,4] as well as pulmonary [5] and heart-related diseases. [6,7]
The H10 trial was groundbreaking, adjusting treatment based on PET scan results after 2 chemotherapy cycles. For patients with a negative scan, radiation therapy (RT) was omitted to avoid long-term side effects. Among patients with favourable prognosis and a negative PET scan, 5-year progression-free survival was 99% with RT after chemotherapy versus 87% with chemotherapy alone, indicating RT necessity. The 10-year follow-up data confirmed that the omission of INRT was associated with lower progression-free survival although no differences in terms of survival emerged.
Conversely, the trial succeeded in showing that patients with a positive PET scan after the first 2 cycles of chemotherapy achieved better outcomes when given an intensified chemotherapy combined with RT. Specifically, the PFS rate at 5 years was 91% for the patients who received intensified combination therapy, versus 77% for those who received standard combination therapy.
The 10-year follow-up data showed no statistically significant differences between standard and intensified therapy in terms of progression-free survival and overall survival.
Early Positron Emission Tomography Response–Adapted Treatment in Stage I and II Hodgkin Lymphoma: Final Results of the Randomized EORTC/LYSA/FIL H10 Trial
Andre MPE, GirinskyT, Federico M, et al.
J Clin Oncol 2017 Jun;35(16):1786-94.
Melanoma
 Melanoma
Melanoma
Melanoma is the deadliest form of skin cancer. Historically, melanoma was a rare cancer, but in the last 50 years its incidence has risen faster than almost any other cancer [1] making it the 19th most commonly occurring cancer worldwide, [2] with over 320,000 new cases and over 55,000 deaths, in 2020. [3] After Australia and New Zealand, European countries have highest rates of melanoma incidence. According to GLOBOCAN, in Europe there are approximately 144.000 cases diagnosed per year and 27.000 deaths related [4].
Starting from pigment-producing cells (melanocytes) in the skin, melanoma spreads to other parts of the body through metastasis. Patients with stage III melanoma usually undergo surgery to remove the primary tumour and the nearby metastasised lymph nodes (i.e., to which mobile tumour cells have migrated). However, successful surgery does not guarantee that patients will be cancer-free, and stage III melanoma patients bear a high risk that their cancer returns.
 Prolonging survival in stage III melanoma – with ipilimumab adjuvant therapy.
Prolonging survival in stage III melanoma – with ipilimumab adjuvant therapy.
Ipilimumab is an antibody-based drug that works as an immune checkpoint inhibitor and thereby increases anti-tumour immune responses. It was approved in 2011 for the treatment of advanced melanoma, at a dose of 3 mg per kilogram of body weight. [1,2]
Based on research suggesting the potential for a higher dose to have higher efficacy (although at a cost of more toxic effects), [3,4] the EORTC 18071 study aimed to evaluate the effect of treating high-risk stage III melanoma patients with ipilimumab at a dose of 10 mg per kilogram – as compared with giving a placebo instead – after surgery to remove their primary tumour and nearby/affected lymph nodes.
The study showed a significant (over 10%) increase in cancer recurrence-free survival with (‘high-dose’) ipilimumab treatment after 5 years, as compared with placebo. [5] Even though there were adverse effects reported with ipilimumab, overall, the drug did not have a negative effect on the patients’ health-related quality of life. [6] After 7 years, ipilimumab still showed durable recurrence-free survival as well as overall survival benefit, with an 8.7% absolute difference for overall survival. [7]
Adjuvant ipilimumab versus placebo after complete resection of stage III melanoma: long-term follow-up results of the European Organisation for Research and Treatment of Cancer 18071 double-blind phase 3 randomised trial.
Eggermont AMM, Chiarion-Sileni V, Grob JJ, et al.
Eur J Cancer 2019 Sep;119:1-10.
 Prolonging recurrence-free survival in stage III melanoma – with pembrolizumab treatment.
Prolonging recurrence-free survival in stage III melanoma – with pembrolizumab treatment.
Pembrolizumab – an antibody-based ‘drug’ – has been shown to stimulate the body’s immune system to remove remaining melanoma cells.
The EORTC KEYNOTE-054 study looked at the effect of treating stage III melanoma patients (after surgery) with pembrolizumab, as compared to giving a placebo instead.
The study showed that pembrolizumab treatment yielded a significant (over 40%) reduction of these patients’ risk of melanoma recurrence or death after 1.25 years. [1]
This outcome led to the approval of pembrolizumab (by EMA in 2018 and FDA in 2019) for use in treating high-risk stage III melanoma patients.
Prolonged recurrence-free survival with this treatment was further confirmed after 3.5 years, with a recurrence-free survival rate of 65% at that point in pembrolizumab-treated patients – which was then 16% higher than with placebo. [2]
Pembrolizumab therapy – given after surgery of the primary tumour – provides a clear and sustained relapse-free survival benefit to stage III melanoma patients and is still considered a viable treatment option to date.
Adjuvant pembrolizumab versus placebo in resected stage III melanoma (EORTC 1325-MG/KEYNOTE-054): distant metastasis-free survival results from a double-blind, randomised, controlled, phase 3 trial.
Eggermont AMM, Blank CU, Mandala M, et al.
Lancet Oncol 2021 May;22(5):643-54.
Soft Tissue & Bone
 Measuring the safety & efficacy of crizotinib in patients with ultra-rare cancers.
Measuring the safety & efficacy of crizotinib in patients with ultra-rare cancers.
Conducting trials in rare cancers is challenging, not least because it is difficult to find enough patients to take part and give a reliable result. Some cancers are so rare that there may only be one or two patients diagnosed in a year in any one country, and even studying existing drugs for use in such a small group is not worthwhile for the pharmaceutical industry. Now, the EORTC CREATE trial is looking at the use of the drug crizotinib in very rare tumours. Crizotinib works by targeting the growth of cancer cells that have specific abnormalities called ALK and MET, and it is already known to be effective in the treatment of advanced lung cancer.
Knowing that ALK and MET abnormalities were involved in some very uncommon cancers, the researchers decided to investigate the effect of crizotinib on six tumour types. The rarity of these cancers can be seen in the fact that fewer than 200 patients in total took part in the trial. Results so far are promising.
For example, in inflammatory myofibroblastic tumours, which occur in smooth muscle and connective tissue cells, researchers have found that the tumours respond well to crizotinib treatment.
The latest results show that up to around 70% of patients have a positive response to treatment, and these data have been used to support an application to the US Food and Drug Administration for the authorisation of the use of crizotinib in children with inflammatory myofibroblastic tumours.
CREATE has been valuable in encouraging the creation of working groups on the ultra-rare tumours being studied and stimulating radiologists as well as medical oncologists to work on them.
Patients in the trial have also benefited from their treatment; many are still on crizotinib even though it is not yet on the market in some countries or in those where it is, it is not approved for the tumour type being studied.
Additionally, the long-term follow-up of the trial will give researchers the chance to better understand the natural course of these rare diseases, and this will aid in the planning of future research.
Long-term efficacy update of crizotinib in patients with advanced, inoperable inflammatory myofibroblastic tumour from EORTC trial 90101 CREATE
Schöffski P, Kubickova M, Wozniak A, et al.
Eur J Cancer 2021 Aug;12(156):12-23.


